Research Article - Journal of Environmental and Occupational Health (2023)
Evaluation of the Effectiveness of Cognitive Behavioural Therapy for Patients Suffering From an Adjustment Disorder
Dominique Jonkers1*, Peter ten Klooster2, Maarten K. van Dijk3, Colin van der Heiden4 and Marc J. P. M. Verbraak52Department of Technology, University of Twente, Enschede, The Netherlands
3Department of Anxiety and Depressive Disorders, Dimence Institute for Specialized Mental Health Care, Deventer, The Netherlands
4Department of Psychology, Erasmus University Rotterdam, Rotterdam, The Netherlands
5Department of Psychology, Radboud University, Nijmegen, The Netherlands
Dominique Jonkers, Department of Personality Disorders, Dimence Institute for Specialized Mental Health Care, Deventer, The Netherlands, Email: d.jonkers@dimence.nl
Received: 24-Apr-2023, Manuscript No. JENVOH-23-96926; Editor assigned: 26-Apr-2023, Pre QC No. JENVOH-23-96926 (PQ); Reviewed: 12-May-2023, QC No. JENVOH-23-96926; Revised: 19-May-2023, Manuscript No. JENVOH-23-96926 (R); Published: 26-May-2023
Abstract
Aim: To investigate the effectiveness of a higher initial dose of sessions in 12 weeks of individual CBT (Cognitive Behavioural Therapy) regarding speeded recovery in patients with an adjustment disorder.
Methods: A pre-post intervention trial conducted among 50 adults treated for AD as the primary diagnosis between November 2011 and December 2012. Patients were randomized to a regular treatment condition (one session each week) or an initial intensive treatment condition (two sessions per week over the first four weeks, one session every two weeks thereafter) to investigate a possible dose-response relationship. The primary outcome measure was psychosocial symptoms (OQ-45). Secondary outcome measures were resumption of work and quality of life (RAND-36). Analyses were performed in 2021-2022.
Results: A significant and large reduction in psychosocial symptoms was found across the two conditions over time (B=-4.0; p<0.001; 95% CI=-5.2 to -2.8; d=1.5). Furthermore, resumption of work (B=0.05; p<0.001) and all aspects of health-related quality of life significantly improved as treatment progressed. Although condition by time interactions were not significant for any of the outcome measures, the intensive treatment condition did show a trend towards a more rapid reduction of psychosocial symptoms in the first four weeks of treatment (between-group d=0.6).
Conclusions: CBT was associated with a large reduction in psychosocial symptoms and improvements in resumption of work and health-related quality of life in AD. Results further suggest a more rapid reduction of symptoms when treatment is delivered in a higher frequency.
Keywords
Adjustment Disorder; AD treatment; psychological treatment; CBT
Introduction
Adjustment disorders (ADs) are described as maladaptive, clinically significant emotional or behavioral symptoms in response to identifiable psychosocial stressors [1]. AD is a common disorder, with prevalence rates ranging from 0.3% to 2.3% in the general population [2-4] to about 11% in patients with psychological complaints seen in community health care [5]. ADs are associated with a risk of developing various severe mental disorders such as anxiety disorders or major depressive disorder [6], suicidality [7-11], and disability in terms of absence from work [12-13]. So far, research into effective treatments for AD is rather limited [14-16].
There are only two systematic reviews on the effects of treatment for AD [17-18]. Studies about psychological treatment for AD were of low quality (i.e., GRADE rankings for the treatment comparisons were low to very low) because of methodological problems such as small sample sizes or lack of appropriate control groups. Despite the scarcity of high quality evidence, some studies do suggest that treatment based on cognitive behavioural principles can be effective in decreasing symptoms of stress and suicidal behaviour and shorten the duration of sickness absence in patients with AD [19-26]. The present study aimed to investigate the effectiveness of individual CBT for patients with AD using an active comparison group. Since untreated AD may increase both the risk of suicide and of developing severe mental disorders, a placebo or waitlist control condition was considered unethical. As the existence of a dose-response relationship on speed of recovery might be considered an alternative plausible indication for the causality of a specific treatment and its outcome in the absence of a placebo control condition [27-28], twelve weekly sessions of CBT (Cognitive Behavioural Therapy) were compared to a condition in which the CBT sessions were delivered more frequently in the initial phase. It was expected that CBT would be associated with significant improvements over 12 weeks in psychosocial symptoms (primary outcome measure), return to work and health-related quality of life (secondary outcome measures). It was further hypothesized that patients in the intensive treatment condition would experience a more rapid reduction of psychosocial symptoms, faster return to work and faster improvement in health-related quality in the first four weeks compared to patients in the regular treatment group.
Materials and Methods
Design
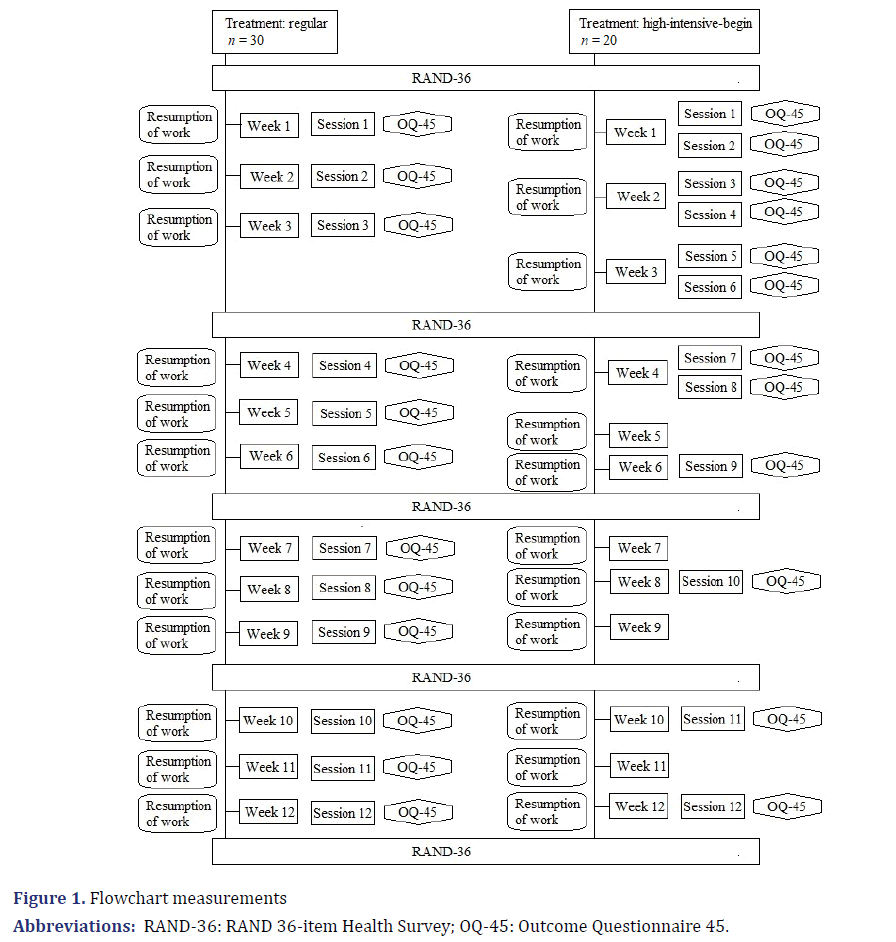
A pre-post intervention trial was conducted among 50 adults treated for AD at the HSK Group, a mental health care centre in the Netherlands. Patients were randomly assigned to either a regular treatment condition (one individual CBT session per week over a period of 12 weeks) or an initial intensive treatment condition (two individual CBT sessions per week over the first four weeks, and one session every two weeks in the subsequent 8 weeks). The study was approved by the Independent Review Board Nijmegen (file number IRBN2010025).
Based on an a priori power analysis with G*Power 3 software version 3.1.9.2 [29-30], the original planning was to recruit 119 patients in total. This power analysis was based on a simple pretest-posttest change in mean psychosocial symptoms in the entire group between baseline and 12 weeks of treatment, without taking any intermediate measures into account. The anticipated minimum effect size was conservatively based on historical observational data on CBT treatment for AD from the HSK group. According to this a-priori power analysis, 119 patients were needed to demonstrate at least a small effect (d=0.23) with a power of 80% and a one-sided α of 0.05. Unfortunately, the study had to be stopped early because health insurance companies in the Netherlands decided to exclude AD from reimbursement, as a result of which referral of patients with AD for treatment ended. In the end, 53 patients were included in the study of which sufficient data was available for 50 patients.
Participants and procedure: Patients were drawn from referrals made by general practitioners to the HSK group. Inclusion criteria were a primary diagnosis of adjustment disorder and age 18-65 [1]. The data was collected from November 2011 to December 2012. Diagnosis was established using the semi-structured Mini International Neuropsychiatric Interview [31-32]. Patients using medication for at least six weeks or longer, were allowed to participate with the requirement to keep the dosage constant in the study period. Only the standard treatment exclusion criteria of the HSK group were maintained, which are: having a psychotic disorder, bipolar disorder, severe substance abuse or severe personality problems (expressed by suicidality or criminality).
All patients participated voluntarily and did not receive financial compensation for their participation. After the diagnosis was established patients were informed about the study by the therapist involved in the intake procedure and received a letter with information. During a second intake interview patients were asked if they were willing to participate. The average time between those two appointments was four days. After signing an informed consent, patients were randomly assigned to one of the two treatment conditions using closed envelopes. Treatment started within two weeks after the second intake interview.
Treatment: Treatments were delivered individually by twelve staff psychologists on six locations of the HSK group. All therapists were master-level psychologists who had received at least a basic training in CBT. All of them had clinical experience in providing manualized cognitive-behavioural treatment. All therapists received additional one-day training in the specific CBT manual for AD by one of the authors (CH) of the treatment manual.
Treatment followed the AD treatment manual consisting of twelve sessions of 45 minutes [33]. During the first phase of treatment (two sessions), information on adjustment disorders and stress reactions is provided, symptoms of stress are monitored as well as the events that trigger increasing levels of stress. Another goal in this first treatment phase is improving lifestyle, by adopting a more healthy lifestyle (e.g., eating pattern, day-night rhythm) and engaging in relaxing and/ or social activities. In the second phase (two sessions) a self-control-program is introduced to help patients to better recognize and deal with rising symptoms of tension. Cognitive restructuring is applied in the fifth to seventh session, aimed at addressing and changing dysfunctional automatic thoughts using Socratic questioning and behavioural experiments. The fourth phase (4 sessions) focuses on strengthening problem solving abilities. In the last session treatment progress is evaluated and a relapse prevention plan is developed.
Measures
The primary outcome was psychosocial symptoms as measured with the total score of the Outcome Questionnaire 45 [34-35]. Patients filled in the OQ-45 prior to each session with respect to how they were doing in the preceding week (Figure 1). All 45 questions are answered on a five point Likert-type scale from “never” to “almost always”. The total score is computed by adding the sum scores of the three subscales “Symptom Distress” (SD; symptoms associated with anxiety and depression), “Interpersonal Relationship” (IR; symptoms associated with feelings of loneliness and social conflicts and difficulties) and “Social Role” (SR; difficulties in occupational settings) with higher scores indicating more severe symptoms. The reliable change index (RCI) for the total score in a patient population is 18 and the best cut-off for discriminating between a normal and patient population is 56 [36]. The OQ-45 has been found to be a psychometrically sound measure to assess treatment effects [37-38].
Secondary outcome measures were resumption of work and health-related quality of life.
Patients’ resumption of work was measured each week as the percentage of hours under contract that a patient had actually worked in a given week, by asking: “How many hours of your contract hours have you been able to work in the past week?”. Health-related quality of life was measured every three weeks using the RAND 36- item Health Survey (RAND-36) [39-40].
This questionnaire assesses eight aspects of health: physical functioning (10 items), social functioning (2 items), role limitations caused by physical health problems (4 items), role limitations caused by emotional problems (3 items), emotional wellbeing (5 items), energy/fatigue (4 items), pain (2 items), and general health perceptions (5 items) and health change (1 item). Psychometric properties of the RAND-36 have been shown to be satisfactory [40-42].
Statistical analysis
Statistical analyses were performed in 2021-2022 with SPSS, version 27 (International Business Machines Corporation IBM, New York, 2020). The balance of background characteristics at baseline across both treatment groups was explored by means of t-tests and chi-square tests as appropriate. Outcome analyses were performed on a modified intention-to-treat basis including all randomized patients who did not withdraw from the study within the first four weeks of treatment.
Treatment effects over time and differences in effects between the two conditions were tested using a series of repeated measures Linear Mixed Models (LMMs) with Restricted Maximum Likelihood (REML) estimation. For patients randomized to the initial intensive group, each second administration of the OQ-45 questionnaire in the first four weeks was used for analysis.
For each outcome measure, a LMM analysis was performed with a random intercept for participants allowing baseline scores to vary between patients. Group, time (week 1-12), and group by time interaction were entered as fixed effects. All models were estimated with an autoregressive AR (1) covariance structure for the repeated measurements as this structure demonstrated the best fit for most outcome measures according to the Akaike and Bayesian information criteria. Assumptions of linearity, normality and homoscedasticity of the residuals were checked using QQ-plots, residual histograms and residuals vs. fitted values plots. The assumptions of homoscedasticity and normality were violated for the secondary outcome measures resumption of work and three RAND-36 subscales (physical functioning, role limitations caused by physical health problems and role limitations caused by emotional problems. Resumption of work was dichotomized into full return to work vs. no full return to work. The three RAND-36 subscales could not be transformed in a meaningful way and their model results need to be interpreted with caution.
For the primary outcome measure (OQ-45 psychosocial symptoms), the proportions of responders (prepost improvement ≥ 18) and remitters (posttest score ≤ 56) in both conditions together were additionally estimated based on available data of study completers.
Results
Descriptives
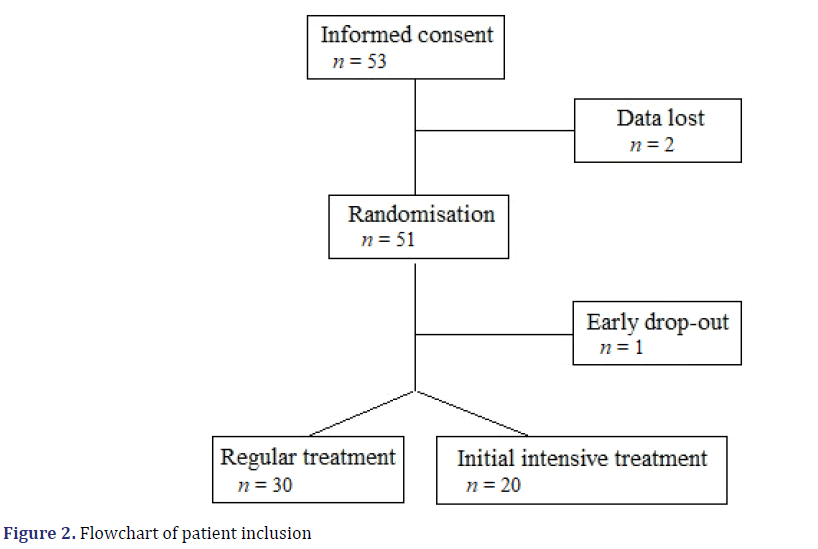
The flowchart of patient inclusion is given in Figure 2. In total, 53 patients were included in the study. Because the study data of two patients were lost for unknown reasons, these patients were excluded from all analyses. Additionally, one patient decided to withdraw participation during the first four sessions of the study. Because most data were missing this patient was also excluded from the analysis of the remaining 50 patients, 30 patients were assigned to the regular treatment condition and 20 were assigned to the initial intensive treatment condition. Ten patients were early completers, i.e., they were able to successfully terminate treatment before the 12th session. Of the 50 patients included for analysis (Table 1), 21 were male and 29 were female with an age between 22 and 63 (M=42.1, SD=11.1). Medication was taken by nine of the 50 patients. Comorbidity was present in six patients. Three patients may have had additional personality problems which were classified as “diagnosis on Axis II postponed”, one patient was additionally diagnosed with a personality disorder, one with a disorder in impulse-control not otherwise specified and one patient suffered from bereavement (not being the cause of AD). The other 44 patients were only diagnosed with AD. The background characteristics did not differ significantly (p<0.05) across both treatment groups.
| Variable | Total (N = 50) |
Regular (n = 30) |
Initial intensive (n = 20) |
pa |
|---|---|---|---|---|
| Age, M (SD) | 42.1 (11.1) | 42.9 (11.4) | 40.8 (10.7) | 0.89 |
| Sex, n (%) | 0.41 | |||
| Male | 21 (42%) | 14 (47%) | 7 (35%) | |
| Female | 29 (58%) | 16 (53%) | 13 (65%) | |
| Treatment ended successfully | 0.47 | |||
| Before 12th session, n (%) | 10 (20%) | 7 (23%) | 3 (15%) | |
| Comorbidity present, n (%) | 6 (12%) | 4 (13%) | 2 (10%) | 0.57 |
| Usage of medication, n (%) | 9 (18%) | 6 (20%) | 3 (15%) | 0.65 |
| Family status, n (%) | 0.96 | |||
| Living alone | 20 (40%) | 12 (40%) | 8 (40%) | |
| Living together | 27 (54%) | 16 (53%) | 11 (55%) | |
| No information | 3 (6 %) | 2 (7%) | 1 (5%) | |
| Education, n (%) | 0.09 | |||
| Low and mid | 29 (58%) | 15 (50%) | 14 (70%) | |
| Higher | 14 (28%) | 11 (37%) | 3 (15%) | |
| No information | 7 (14%) | 4 (13%) | 3 (15%) | |
| Previous psychological treatment, | 18 (36%) | 0.58 | ||
| n (%) | 7 (14%) | |||
| Yes | 10 (33%) | 8 (40%) | ||
| No information | 4 (13%) | 3 (15%) |
Note: aFor age an independent-samples t-test was used, for the rest of the variables chi-square tests were used.
Primary outcome measure
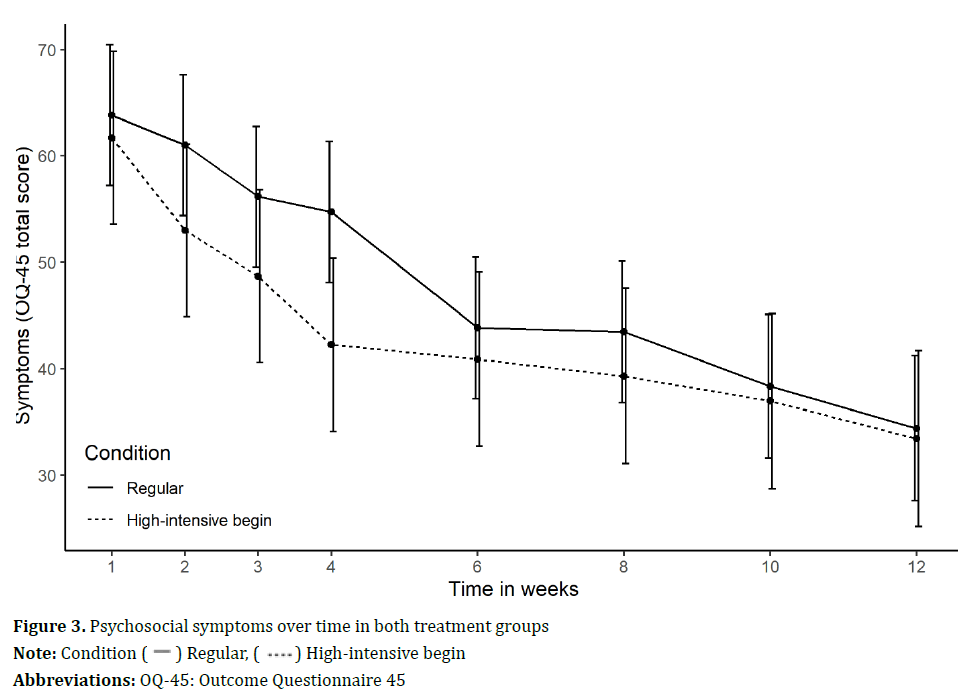
LMM analyses revealed a significant effect of time (n=50; F=108.6; p<0.001), indicating an overall significant reduction in psychosocial symptoms across the two groups over time. The within-group effect over 12 weeks was large (Cohen’s d=1.5). At post-treatment, 64% patients could be classified as treatment responders and 62% could be classified as remitters. There was no significant effect of condition (F=0.6; p=0.46), indicating no average difference in psychosocial symptoms between the groups over all weeks. There was also no significant interaction effect (F=0.1; p=0.79) for the primary outcome measure, indicating that the change in psychosocial symptoms did not significantly differ between the two groups over time (Table 2). However, the estimated marginal means did show a clear trend in that patients in the initial intensive treatment condition experienced a more rapid reduction of psychosocial symptoms in the first weeks of treatment (Figure 3). The between-group difference after four weeks of treatment was moderate in size (Cohen’s d=0.6).
| Week | Group M (SE) |
Fixed effects estimates (95% CI) |
|||
|---|---|---|---|---|---|
| Regular (n = 30) |
Initial intensive (n = 20) |
Group | Time | Group × Time | |
| 1 | 63.8 (3.3) | 61.7 (4.1) | 4.2 (7.1 to15.4) | -4.0 (-5.2 to 2.8)*** | -0.2 (-1.8 to 1.4) |
| 2 | 61.0 (3.3) | 53.0 (4.1) | |||
| 3 | 56.2 (3.3) | 48.7 (4.1) | |||
| 4 | 54.7 (3.3) | 42.3 (4.1) | |||
| 6 | 43.8 (3.4) | 40.9 (4.1) | |||
| 8 | 43.5 (3.4) | 39.3 (4.1) | |||
| 10 | 38.3 (3.4) | 37.0 (4.2) | |||
| 12 | 34.4 (3.4) | 33.4 (4.2) | |||
Note: ***p<0.001, OQ-45 = Outcome Questionnaire 45
Secondary outcome measures
An overall significant effect of time was also found for resumption of work (n=46; F=20.3; p<0.001) and all aspects of health-related quality of life (n=50; physical functioning: F=30.2, p<0.001; role limitations caused by physical health problems: F=53.1, p<0.001; role limitations caused by emotional problems: F=64.6, p<0.001; energy/fatigue: F=84.7, p<0.001; emotional wellbeing: F=105.1, p<0.001; social functioning: F=76.8, p<0.001; pain: F=21.1, p<0.001; general health perceptions: F=24.8, p<0.001). Across the two conditions significantly more patients were able to work all their contract hours and all aspects of health-related quality of life improved as treatment progressed. There was no significant effect of condition for health-related quality of life except for the RAND-36 subscale ‘role limitations caused by physical health problems’ (F=3.9, p=0.05). There was no significant group by time interaction effects for any of the secondary outcomes (Table 3). Patients in the initial intensive treatment condition did not appear to experience a faster return to work, nor a faster improvement in health-related quality of life compared to patients in the regular treatment group.
| Outcome | Week | Group M (SE) |
Fixed effects estimates (95% CI) | |||
|---|---|---|---|---|---|---|
| Regular (n = 30) | Initial intensive (n = 20) |
Group | Time | Group × Time | ||
| Resumption of work (binary)a | 1 | 0.4 (0.1) | 0.3 (0.1) | -0.005 (-0.3 to 0.3) | 0.05 (0.01 to 0.08)** | 0.002 (-0.04 to 0.05) |
| 2 | 0.3 (0.1) | 0.3 (0.1) | ||||
| 3 | 0.4 (0.1) | 0.3 (0.1) | ||||
| 4 | 0.4 (0.1) | 0.3 (0.1) | ||||
| 6 | 0.3 (0.1) | 0.3 (0.1) | ||||
| 8 | 0.5 (0.1) | 0.5 (0.1) | ||||
| 10 | 0.5 (0.1) | 0.5 (0.1) | ||||
| 12 | 0.8 (0.1) | 0.8 (0.1) | ||||
| RAND-36 PF | 0 | 84.0 (2.3) | 88.3 (2.8) | -5.6 (-13.7 to 2.5) | 1.8 (0.5 to 3.0)** | 1.1 (-0.6 to 2.7) |
| 3 | 85.8 (2.3) | 91.8 (2.8) | ||||
| 6 | 89.5 (2.3) | 92.2 (2.9) | ||||
| 9 | 91.6 (2.3) | 94.4 (2.9) | ||||
| 12 | 95.4 (2.4) | 95.2 (2.9) | ||||
| RAND-36 RP | 0 | 37.1 (6.7) | 51.3 (8.2) | -23.9 (-47.7 to -0.07)* | 9.2 (4.5 to 13.9)*** | 3.9 (-2.2 to 10.0) |
| 3 | 45.1 (6.7) | 70.0 (8.2) | ||||
| 6 | 64.8 (6.7) | 78.7 (8.3) | ||||
| 9 | 67.6 (6.9) | 82.2 (8.4) | ||||
| 12 | 89.2 (7.0) | 90.4 (8.4) | ||||
| RAND-36 RE | 0 | 18.8 (7.2) | 33.3 (8.7) | -13.0 (-37.6 to 11.7) | 10.3 (5.5 to 15.1)*** | 4.7 (-1.6 to 11.0) |
| 3 | 43.9 (7.2) | 43.3 (8.7) | ||||
| 6 | 63.0 (7.2) | 47.0 (8.9) | ||||
| 9 | 58.2 (7.4) | 65.6 (9.0) | ||||
| 12 | 83.9 (7.5) | 74.0 (9.0) | ||||
| RAND-36 VT | 0 | 43.3 (3.0) | 45.3 (3.7) | -2.5 (-13.5 to 8.4) | 5.8 (3.8 to 7.9)*** | 0.6 (-2.1 to 3.3) |
| 3 | 49.6 (3.0) | 49.0 (3.7) | ||||
| 6 | 54.7 (3.0) | 56.3 (3.7) | ||||
| 9 | 59.6 (3.1) | 61.9 (3.7) | ||||
| 12 | 69.4 (3.1) | 68.6 (3.7) | ||||
| RAND-36 MH | 0 | 52.9 (2.7) | 56.2 (3.3) | -2.4 (-12.1 to 7.2) | 5.2 (3.5 to 6.8)*** | 0.6 (-1.6 to 2.7) |
| 3 | 58.6 (2.7) | 56.4 (3.3) | ||||
| 6 | 64.0 (2.7) | 62.0 (3.4) | ||||
| 9 | 68.1 (2.8) | 69.3 (3.4) | ||||
| 12 | 76.0 (2.8) | 76.6 (3.4) | ||||
| RAND-36 SF | 0 | 59.2 (3.1) | 59.4 (3.8) | -0.4 (-11.8 to 10.9) | 5.8 (3.5 to 8.1)*** | 1.7 (-1.3 to 4.7) |
| 3 | 68.5 (3.1) | 64.4 (3.8) | ||||
| 6 | 77.0 (3.2) | 67.3 (3.9) | ||||
| 9 | 81.2 (3.2) | 76.7 (3.9) | ||||
| 12 | 89.5 (3.3) | 82.8 (3.9) | ||||
| RAND-36 BP | 0 | 72.7 (3.45) | 68.3 (4.2) | 2.7 (-9.6 to 15.0) | 3.4 (1.0 to 5.8)** | 0.2 (-2.8 to 3.3) |
| 3 | 70.5 (3.47) | 71.6 (4.2) | ||||
| 6 | 78.5 (3.48) | 75.4 (4.3) | ||||
| 9 | 82.0 (3.56) | 78.1 (4.3) | ||||
| 12 | 86.5 (3.59) | 82.2 (4.3) | ||||
| RAND-36 GH | 0 | 66.1 (2.9) | 64.5 (3.6) | 2.3 (-7.6 to 12.1) | 3.0 (1.5 to 4.5)*** | -1.2 (-3.1 to 0.8) |
| 3 | 65.0 (2.9) | 66.4 (3.6) | ||||
| 6 | 69.5 (2.9) | 71.3 (3.6) | ||||
| 9 | 69.8 (3.0) | 71.7 (3.6) | ||||
| 12 | 73.2 (3.0) | 76.6 (3.7) | ||||
Note: *p<0.05; **p<0.01; ***p<0.001, an = 28 for regular group and n = 18 for initial intensive group
Abbreviations: RAND-36: RAND 36-item Health Survey; PF: Physical Functioning; RP: Role-Physical; RE: Role-Emotional; VT: Vitality; MH = Mental Health; SF: Social Functioning; BP: Bodily Pain; GH: General Health
Discussion
The main goal of this study was to examine whether CBT is an effective treatment for adjustment disorder. By randomly assigning patients to either a regular treatment condition (12 weekly sessions) or an initial intensive treatment condition (two sessions per week over the first four weeks, and biweekly sessions in the subsequent 8 weeks) additionally the presence of a dose-response relationship was explored. An overall significant and large reduction in psychosocial symptoms was found across the two groups. At post-treatment 64% of patients could be classified as treatment responders, 62% as remitters. Furthermore, across the two groups; significantly more patients were able to fully return to work and health-related quality of life improved as treatment progressed. These results are in line with the results of other studies suggesting that CBT is an effective treatment for patients with AD [19- 26]. Contrary to expectations, a high initial frequency of treatment sessions was not found to result in significantly stronger improvements over the 12 weeks as compared to weekly sessions on any of the outcome measures. However, it should be noted that this assumption was only statistically tested with a linear group by time interaction term assuming linear changes over the entire 12 weeks of treatment. Visual inspection of the mean psychosocial symptoms scores across both conditions did show a clear trend towards a more rapid reduction of symptoms in the first four weeks of treatment with a moderate between-group effect size. This dose-response effect was not clearly visible in any of the secondary outcomes, which could be because it is usually the case that you first recover from complaints before you can resume your work and the quality of life increases. These secondary outcome measures may be less sensitive to a more speedy change.
To our knowledge, this is the first treatment study for AD testing the existence of a dose-effect of psychotherapy. One limitation of this study is the sample size, for reasons discussed in section ‘Design’. Partly for this reason, we did not perform extensive post-hoc analyzes or otherwise test the dose-response effect. Further studies with larger sample sizes also enabling more sophisticated statistical analyses are needed to reach more definitive conclusions on this topic. A second limitation is the violations of the residual normality, linearity and homoscedasticity assumptions of the LMM analysis for some of the secondary outcome measures. It was not possible to transform these variables and meaningful cut-off points for dichotomization are not known. Therefore, care should be taken in interpreting the results.
Conclusion
In summary, the present study provides an additional indication that CBT might be effective in treating AD patients in terms of improvement in psychosocial symptoms, work status and health-related quality of life. However, further research is needed to investigate whether there is a causal relationship between offering CBT treatment and improvement in psychosocial symptoms, work status and health-related quality of life. Outcomes of a Randomized-Controlled Trial (RCT) with a placebo control group and a large sample size could provide the strongest evidence for such a causal relationship but unfortunately it is complicated to conduct such a study in clinical practice because of the ethical objections not to offer treatment to patients with such serious problems classified as AD.
References
- American Psychiatric Association APA. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Revision (DSM-IV-TR) Washington DC: 2001.
- Fernández A, Mendive JM, Salvador-Carulla L, Rubio-Valera M, Luciano JV, Pinto-Meza A, et al. Adjustment disorders in primary care: prevalence, recognition and use of services. Br J Psychiatry 2012;201:137-142.
[Crossref] [Google scholar] [Pubmed]
- Lejtzén N, Sundquist J, Sundquist K, Li X. Depression and anxiety in Swedish primary health care: prevalence, incidence, and risk factors. Eur Arch Psychiatry Clin Neurosci 2014;264:235-245.
[Crossref] [Google scholar] [Pubmed]
- Semaan W, Hergueta T, Bloch J, Charpak Y, Duburcq A, Le Guern ME, et al. Cross-sectional study of the prevalence of adjustment disorder with anxiety in general practice. Encephale 2001;27:238-244.
[Google scholar] [Pubmed]
- Shear MK, Greeno C, Kang J, Ludewig D, Frank E, Swartz HA, et al. Diagnosis of nonpsychotic patients in community clinics. Am J Psychiatry 2000;157:581-587.
[Crossref] [Google scholar] [Pubmed]
- O’Donnell ML, Alkemade N, Creamer M, McFarlane AC, Silove D, Bryant RA, et al. A longitudinal study of adjustment disorder after trauma exposure. Am J Psychiatry 2016;173:1231-1238.
[Crossref] [Google scholar] [Pubmed]
- Casey P, Maracy M, Kelly BD, Lehtinen V, Ayuso-Mateos JL, Dalgard OS, et al. Can adjustment disorder and depressive episode be distinguished? Results from ODIN. J Affect Disord 2006;92:291-297.
[Crossref] [Google scholar] [Pubmed]
- Casey P, Jabbar F, O’Leary E, Doherty AM. Suicidal behaviours in adjustment disorder and depressive episode. J. Affect. Disord 2015;174:441-446.
[Crossref] [Google scholar] [Pubmed]
- Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Lash TL. The association between adjustment disorder diagnosed at psychiatric treatment facilities and completed suicide. Clin Epidemiol 2010;2:23-28.
[Crossref] [Google scholar] [Pubmed]
- Kryzhanovskaya L, Canterbury R. Suicidal behavior in patients with adjustment disorders. Crisis 2001; 22:125-131.
[Crossref] [Google scholar] [Pubmed]
- Pelkonen M, Marttunen M, Henriksson M, Lönnqvist J. Suicidality in adjustment disorder--clinical characteristics of adolescent outpatients. Eur Child Adolesc Psychiatry 2005; 14:174-180.
[Crossref] [Google scholar] [Pubmed]
- Catalina-Romero C, Pastrana-Jiménez JI, Tenas-López MJ, Martínez-Muñoz P, Ruiz-Moraga M, Fernández-Labandera C, et al. Long-term sickness absence due to adjustment disorder. Occup Med 2012;62:375-378.
[Crossref] [Google scholar] [Pubmed]
- Koopmans PC, Bültmann U, Roelen CA, Hoedeman R, van der Klink JJ, Groothoff JW. Recurrence of sickness absence due to common mental disorders. Int Arch Occup Environ Health 2011;84:193-201.
[Crossref] [Google scholar] [Pubmed]
- Kazlauskas E, Zelviene P, Lorenz L, Quero S, Maercker A. A scoping review of ICD-11 adjustment disorder research. Eur J Psychotraumatol 2017;8:1421819.
[Crossref] [Google scholar] [Pubmed]
- O’Donnell ML, Agathos JA, Metcalf O, Gibson K, Lau W. Adjustment disorder: current developments and future directions. Int J Environ Res Public Health 2019;16:2537.
[Crossref] [Google scholar] [Pubmed]
- Zelviene P, Kazlauskas E. Adjustment disorder: current perspectives. Neuropsychiatr Dis Treat 2018;14:375-381.
[Crossref] [Google scholar] [Pubmed]
- Constantin D, Dinu EA, Rogozea L, Burtea V, Leasu FG. Therapeutic interventions for adjustment disorder: a systematic review. Am J Ther 2020;27:e375-e386.
[Crossref] [Google scholar] [Pubmed]
- O’Donnell ML, Metcalf O, Watson L, Phelps A, Varker T. A systematic review of psychological and pharmacological treatments for adjustment disorder in adults. J Trauma Stress 2018;31:321-331.
[Crossref] [Google scholar] [Pubmed]
- Dalgaard L, Eskildsen A, Carstensen O, Willert MV, Andersen JH, Glasscock DJ. Changes in self-reported sleep and cognitive failures: A randomized controlled trial of a stress management intervention. Scand J Work Environ Health 2014;40:569-581.
[Crossref] [Google scholar] [Pubmed]
- Leterme AC, Behal H, Demarty AL, Barasino O, Rougegrez L, Labreuche J, et al. A blended cognitive behavioral intervention for patients with adjustment disorder with anxiety: a randomized controlled trial. Internet Interv 2020;21:100329.
[Crossref] [Google scholar] [Pubmed]
- Quero S, Molés M, Campos D, Andreu-Mateu S, Baños RM, Botella C. An adaptive virtual reality system for the treatment of adjustment disorder and complicated grief: 1-year follow-up efficacy data. Clin Psychol Psychother 2019;26:204-217.
[Crossref] [Google scholar] [Pubmed]
- Ruesch M, Helmes A, Bengel, J. Cognitive behavioral group therapy for patients with physical diseases and comorbid depressive or adjustment disorders on a waiting list for individual therapy: results from a randomized controlled trial. BMC psychiatry 2017;17:340.
[Crossref] [Google scholar] [Pubmed]
- Sanz Cruces JM, García Cuenca IM, Lacomba-Trejo L, Cuquerella Adell MÁ, Cano Navarro I, Ferrandis Cortés M, et al. Group therapy for patients with adjustment disorder in primary care. Span J Psychol 2018;21: e50.
[Crossref] [Google scholar] [Pubmed]
- van der Heiden C, Melchior K. Cognitive-behavioral therapy for adjustment disorder: a preliminary study. ABCT 2012;35:57-60.
- van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. The benefits of interventions for work-related stress. Am J Public Health 2001;91:270-276.
[Crossref] [Google scholar] [Pubmed]
- van der Klink JJL, Blonk RWB, Schene AH, van Dijk FJH. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Int J Occup Environ Health 2003;60:429-437.
[Crossref] [Google scholar] [Pubmed]
- Höfler M. The Bradford Hill considerations on causality: a counterfactual perspective. Emerg. Themes Epidemiology. 2005;2.
[Crossref] [Google scholar] [Pubmed]
- Shapiro S. Causation, bias and confounding: a hitchhiker’s guide to the epidemiological galaxy Part 3: Principles of causality in epidemiological research: statistical stability, dose- and duration-response effects, internal and external consistency, analogy and biological plausibility. J Fam Plann Reprod Health Care 2008;34:261-264.
[Crossref] [Google scholar] [Pubmed]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-191.
[Crossref] [Google scholar] [Pubmed]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41:1149-1160.
[Crossref] [Google scholar] [Pubmed]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22-33.
[Google scholar] [Pubmed]
- van Vliet IM, Leroy H, van Megen HJGM. M.I.N.I Plus: M.I.N.I. Internationaal Neuropsychiatrisch Interview. Nederlandse versie 5.0.0.
- Van der Heiden C, Verbraak MJPM. Behandelprotocol bij aanpassingsstoornissen; Therapeutenboek & Werkboek. Amsterdam: Boom. 2010.
- Lambert MJ, Hanssen NB, Umphress V, Lunnen K, Okiishi J, Burlingame GM, et al. Administration and scoring manual for the Outcome Questionnaire (OQ–45.2). Wilmington: American Professional Credentialing Services 1996.
- de Jong K, Nugter MA, Lambert MJ, Burlingame GM. Handleiding voor afname en scoring van de Outcome Questionnaire (OQ-45). Salt Lake City UT: OQ Measures; 2009.
- Timman R, de Jong K, de Neve-Enthoven N. Cut-off scores and clinical change indices for the Dutch Outcome Questionnaire (OQ-45) in a large sample of normal and several psychotherapeutic populations. Clin Psychol Psychother 2017;24:72–81.
[Crossref] [Google scholar] [Pubmed]
- Boswell DL, White JK, Sims WD, Harrist RS, Romans JSC. Reliability and validity of the Outcome Questionnaire-45.2. Ment Health Phys 2013;112:689-693.
- de Jong K, Nugter MA, Polak M, Wagenborg H, Spinhoven P, Heiser W. De Nederlandse versie van de Outcome Questionnaire (OQ-45): een crossculturele validatie. Psychol Health 2008;36:35-45.
- Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-483.
[Google scholar] [Pubmed]
- van der Zee KI, Sanderman R. Het meten van de algemene gezondheidstoestand met de RAND-36, een handleiding. Tweede herziene druk. UMCG/Rijksuniversiteit Groningen, Research Institute SHARE; 2012.
- van der Zee KI, Sanderman R, Heyink J. A comparison of two multidimensional measures of health status: The Nottingham Health Profile and the RAND 36-Item Health Survey 10. Qual Life Res 1996;5:165-174.
[Crossref] [Google scholar] [Pubmed]
- van der Zee KI, Sanderman R, Heyink JW, de Haes H. Psychometric qualities of the RAND 36-item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med 1996;3:104-122.
[Crossref] [Google scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.





 ) Regular, (
) Regular, ( ) High-intensive begin
) High-intensive begin